
DISCLAIMER
Please note: The information contained in this section is restricted to medical and healthcare practitioners for general education and information purpose only

Body temperature refers to the temperature in the hypothalamus and the vital intense organs. The hypothalamus regulates the body temperature. It checks the current temperature and compares it with the normal temperature of about 98.6°F. If the temperature is too low, the hypothalamus ensures that the body generates and maintains heat. If, on the other hand, the current body temperature is too high, heat is given off, or sweat is produced to cool the skin. People develop fever due to an increase in the hypothalamic set point as an adaptive response of the body to a pathological state. Hyperthermia on the other hand, is an abnormally high temperature (above 104°F) also known as overheating. Hyperthermia occurs without an increase in the hypothalamic set point and the body temperature becomes elevated due to thermoregulation failure.
Reference: InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-
How does the urinary system work?2009 Nov 25 [Updated 2018 Apr 5]
Fever is “a physiologic response characterized by an elevation of body temperature above normal daily variation”. Below are the pathophysiologic bases of fever:
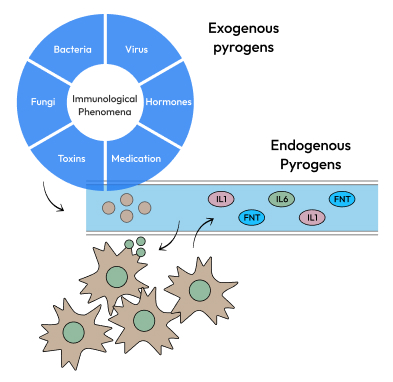
Fever is the result of a physiological process triggered by an external stimulus. Pyrogens (exogenous and endogenous) are substances which may be infectious microorganisms, toxins released by microorganisms, or pyrogenic cytokines that prompt fever.

Exogenous pyrogens, like microbial pyrogens- bacteria, virus, fungi, start the cycle by stimulating host cells, especially macrophages, to produce and release endogenous pyrogenic cytokines like IL-1ẞ.
Endogenous pyrogens trigger the synthesis of prostaglandins (PGs) which act on the hypothalamus, and raises the thermostatic set point to initiate the febrile response. Of all the PGs, PGE2 are the key mediators involved in fever pathogenesis.
The major fever causing cytokines are IL-1β, IL-1α, IL-6, TNF-α and INF-α. These cytokines can be produced in the periphery and brain and have a pyrogenic effect directly affecting the production of PGE2, which resets the thermoregulatory set point.
An early rapid phase (peripheral prostaglandin E2 [PGE2]-dependent) and a delayed late phase (central PGE2) mark the febrile response. Hence, while peripheral PGE2 may act to initiate the febrile response, central PGE2 may be mostly involved in its sustenance.
The humoral pathway is directed by circulating pyrogenic cytokines (IL-1β, IL-6, tumor necrosis factor [TNF]-α). They send fever indicators to the thermoregulatory network through indirect and direct routes. The indirect pathway includes binding cytokines outside the brain and stimulating the cytokine receptors located on the capillaries of the circumventricular organ resulting in PGE2 release. The direct pathway involves disruption of the blood-brain barrier by the circulating cytokines giving direct access to cytokine receptors present on vascular, glial, and neuronal structures of the brain.
While PGE2 is essential in the febrile response, certain cytokines, such as IL-6, may also trigger the febrile response independent of PGE2.
In the neuronal pathway, peripheral nerves such as the cutaneous sensory and vagus nerve are involved. Localized PGE2 synthesized at inflammation sites may activate cold-sensitive cutaneous nerves, transmitting fever signals to the brain.
Reference: Gambhir A, Tamboli S, Prasad S, Inamdar NR. Pyrogenic cytokines mediated pathophysiology of fever and role of
Mefenamic Acid in pediatric practice. Indian Journal of Clinical Practice. 2021; 32: 229-236.
NLRP3 inflammasome activation The Nod-like receptor protein-3 (NLRP3) inflammasome has been implicated in several acute and chronic human diseases. The NLRP3 inflammasome is known to sense disturbances in cellular homeostasis for its activation. Multiple cellular signals that have divergent molecular characterization can trigger NLRP3 activation.
Two signals activate NLRP3 inflammasome; one is via activation of nuclear factors-κβ by Pathogen assisted molecular pattern (PAMPs) and Damage associated molecular patterns (DAMPs)and formation of pro-IL1β.
NLRP3 induces ionic flux events in treated cells, including K+ efflux, Ca2+ mobilization, Cl-1 efflux, and Na+ influx, which are implicated in activating the NLRP3 inflammasome. Activation of NLRP3 inflammasome leads to the release of IL-1β and other pyrogenic cytokines. These pyrogenic cytokines act in the brain to augment the synthesis of cyclooxygenase enzyme increasing the production of PGE2s thus causing fever.
Aberrant activation of the microglial/NLRP3 inflammasome/IL-1 axis has been implicated in the febrile illness epilepsy syndrome (FIRES), which creates a pro-
inflammatory and pro-convulsive milieu
Classification of acute febrile illness



Clinically described fever patterns can be helpful in indicating the possible causes of infections.
| Categories | Fever type | Fever Pattern | |||
|---|---|---|---|---|---|
| Acute fever (<7 days) | Sub-acute fever (usually not more than two weeks in duration) | Chronic or persistent fevers (>2 weeks duration) | Sustained or continuous fever (fever that oscillates less than 1-5°F daily, doesn’t touch normal) |
Remittent fever (fever that falls to normal each day) |
|
| URTI |  |
 |
|||
| COVID-19 |  |
 |
|||
| Dengue |  |
 |
|||
| Chikungunya |  |
 |
|||
| Malaria |  |
 |
|||
| Typhoid |  |
 |
 |
||
| Tuberculosis |  |
 |
|||
| Typhus |  |
 |
|||
| Urinary tract infection |  |
 |
|||

